Major leaps in medical technology frequently inspire both awe and hope. But the public, and even caregivers, often are left gazing up from the launch pad, unsure of how they can best benefit from perceived progress.
With each new advance people expect better health care yet don’t know where to find it. The recent rise of managed care has led to better treatment in some cases, but uncertainty in others. Hospitals – once seen as bedrock institutions – have downsized, declared bankruptcy or, in many cases, closed altogether. Whether neophytes or pioneers, how do individuals who work in the health care industry negotiate hurdles and spur progress in a field that continues to redefine itself? That’s just one question we asked the following Wharton graduates who have embraced the challenges of health care. Their answers help explain what it takes to survive in a field whose priorities and rules are constantly shifting.
 H.L. Perry Pepper: Reinventing a Hospital
H.L. Perry Pepper: Reinventing a Hospital
In almost 25 years as CEO of Chester County Hospital, H.L. Perry Pepper, WG’73, has blazed through battles with HMOs, fended off acquisitions and developed affiliations with other hospitals all while building on the services and infrastructure of his own. “It’s all part of a wonderful, wild ride,” says Pepper. “It’s been a new hospital every year.” Now 58, he was just 34 years old when he started his career as CEO here. Decades later, and despite many offers to leave, he says he wouldn’t dream of working anywhere else. “I’m having too much fun growing and developing the hospital. I don’t remember a time when the job of being a health care provider wasn’t complicated. But I found I had the personality to deal with changes and problems – you develop a vision that extends over quite a period of time.”
Pepper left the marketing division of Smith Kline & French Laboratories (now GlaxoSmithKline) after working there for two years because he wanted “to see what this thing called health care was all about.” Already armed with a sociology degree from the University of Pennsylvania, Pepper then earned his MBA in Health Care Economics from Wharton in 1973. Many of his classmates, he says, were headed for consulting and managed care firms.
“There were very few of us interested in hospital administration. What changed my mind was that I was lucky enough to get a summer residency at the Presbyterian-University of Pennsylvania Medical Center.” After just one summer, he had decided on his future. “I had a full-blown case of health care provider interest and became very interested in the clinical delivery of medicine.”
Asked to become assistant director at Presbyterian in 1973 he accepted and stayed for four years. “It was so different from my corporate experience. When I got into health care I was stimulated by the moment-to-moment variability of the field – the clinical changes and the academic and political milieu. It was the right place for me.”
Pepper channeled that passion – and a vision – to Chester County Hospital (CCH) when he arrived in 1977. “I so deeply believe in a community’s identification with its hospitals and [feel strongly] that a community should govern its health care institution. Of course, this is a not-for-profit, so the shareholders are the community and our charitable goal is to return value in the provision of quality services,” says Pepper. Located in one of the fastest-growing suburban counties of the Philadelphia region, the 108-year-old hospital has continued to build on its services and keep up with the changing needs of the community.
Growing a staff of providers who share his vision, and respect one another’s work, has been a crucial part of Pepper’s plan. But allowing them to find their own strengths is just as important. “It’s putting the bits and pieces of a puzzle together.” The medical staff development at CCH, as well as development of affiliations with other hospitals and specialty programs, have helped redefine the institution.
“We lived through managed care and we avoided being acquired because we could mix and match our affiliations in a way that was good for the community.” Pepper explains.
In 1994, it seemed he was actually pitted against his alma mater, the University, which appeared positioned to acquire the hospital. At that time, large hospital systems were convinced that in order to succeed in managed care contracting they needed to acquire regional hospitals and doctors. “We were the fertile territory to be settled, and suddenly we had people coming out to settle us. In the end, fully capitated managed care proved unpopular because the public didn’t want to be channeled; they liked choice. When the Allegheny system began to unravel, the battle fizzled in favor of CCH.
“It was a difficult period where we had to fight back and not miss the boat in terms of partnering in managed care contracting. We held our ground, however, and happily we convinced the University that being simply a contractual affiliate was better for both of us.”
Positioned in the heart of the thriving community that stretches past the choked borders of the 202 corridor, CCH continues to thrive. Between 1999 and 2004 Pepper anticipates a six percent growth in services and clients. Pepper says the need for health care has been vastly underestimated. “People are living longer and demanding more.” Despite the changing face of this Chester County community, he’s confident CCH can maintain its intimate bond with the residents it serves. “It’s a matter of intent, focus and making yourself available. You can be big, but you can also keep the foundations of a primary relationship. I would try to stop the growth if I felt we were losing that relationship.”
John M. Eisenberg: Feeling Patients’ Pain
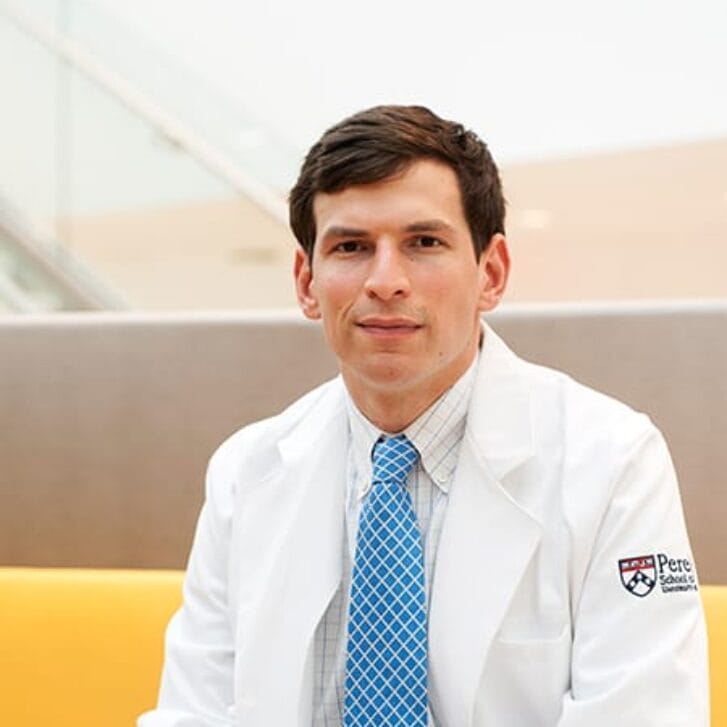
Dr. John M. Eisenberg, WG’76, acknowledges that there are many diseases left to be cured and epidemics to be solved, but as director of the Agency for Healthcare Research and Quality (AHRQ) for the last four years, his has been an even more basic medical mission.
“What the agency’s mission has been of late is improving the quality of health care and measuring the improvement of that quality of care,” says Eisenberg from his home in suburban Maryland. “We are looking at the broader issue of optimizing health care in this country.”
 Eisenberg has spent most of his medical career investigating ways to improve how health care is administered. When he was an undergraduate at Princeton University, he studied under Professors Ann and Herman Somers, who were doing seminal research in basic patient care, and he continued the interest at Washington University Medical School. He then came to the University of Pennsylvania health system as a resident and won a Robert Wood Johnson Foundation fellowship to stay on at the system and, meanwhile, get his MBA at Wharton.
Eisenberg has spent most of his medical career investigating ways to improve how health care is administered. When he was an undergraduate at Princeton University, he studied under Professors Ann and Herman Somers, who were doing seminal research in basic patient care, and he continued the interest at Washington University Medical School. He then came to the University of Pennsylvania health system as a resident and won a Robert Wood Johnson Foundation fellowship to stay on at the system and, meanwhile, get his MBA at Wharton.
“I realized you could do research and be an outstanding physician as well,” says Eisenberg. “I wanted to learn to make the bridge between the clinical and health care systems. Penn was a special place then because it was a cauldron for this new field that was developing.”
Though he became chief of the division of General Internal Medicine at Penn, Eisenberg continued to make the efficiency of health care a priority. He wrote dozens of journal articles on the subject as well as the book, Doctors’ Decisions and the Cost of Medical Care. Eventually, he came to Washington to help put his expertise to work in the federal government. (The AHRQ is part of the U.S. Department of Health and Human Services.)
Eisenberg feels decent strides have been made in recent years in general patient care. He points to new rules by accreditation agencies and some states mandating hospitals and other health care facilities to monitor patients’ pain on a steady basis as one good step. But he knows there is a long way to go.
“One of the things we have worked on very hard is developing a way in which outcomes of care can be measured, so we can associate those outcomes with interventions,” he says. “The general consensus, though, is that research on health care delivery has been neglected. Of course, we need to continue biologic research. But we need to continue this, too. Without better communications between patients and doctors, we are not going to be providing efficient care.”
Eisenberg doesn’t view the change in presidential administrations in Washington as affecting his work. “I continue to hope that we get the kind of recognition we need to get funding for this research,” he says, mentioning that both U.S. Sen. Arlen Spector, a Republican from Pennsylvania, and U.S. Sen. John Breaux, a Democrat from Louisiana, have been leaders in helping research for health care delivery. “What we can expect to get from this kind of research is to improve knowledge about the relationship between the care provided and what outcomes people actually get,” he says. “We have to improve the decisions doctors make. We have to learn how to provide health care at a reasonable cost.”
“If we can solve these problems with rigorous research, we will have a health care system that is even more effective than it is today,” he says. “The goal is to have more successes with higher quality and fewer errors. For even if you have great biologic cures, if you can’t deliver them efficiently, all the work behind them can be lost.”
While the explosion of medical information primarily is a good thing, says Eisenberg, it is not a panacea in itself for medical care. “The point is for clinicians and patients to communicate. That is where quality health care happens,” he says. “Information on the Internet is fine, but we still need to have research on basic care.”
Blaise Judja- Sato: The Fed Ex of Remote Medical Care
When Blaise Judja-Sato, WG’94, looks back at his native Africa, he sees potential wasted. But unlike others in business, he has not looked for ways to exploit the continent’s vast natural resources or searched for niche markets for some product. Judja-Sato, who has had a long history of success in the telecommunications business since getting his Wharton MBA, is instead enthralled with making basic vaccines and essential drugs available to even the most remote citizens of Africa.
 With the support of a number of big-name foundations, he has started VillageReach, which he says will “provide that last mile, to guarantee that vaccines to save lives will get to kids wherever they live – be it the jungle or in remote villages or in the squalor of cities.”
With the support of a number of big-name foundations, he has started VillageReach, which he says will “provide that last mile, to guarantee that vaccines to save lives will get to kids wherever they live – be it the jungle or in remote villages or in the squalor of cities.”
A native of Cameroon who was educated in Africa and France before coming to Wharton, Judja-Sato worked for AT&T in international business development, helping build the undersea cable Africa One, which loops around the continent connecting all its nations. He then signed on as director of international development for Teledesic, a Seattle-based satellite broadband technology company created by tech giants Bill Gates and Craig McCaw.
But in the meantime, Judja-Sato decided to reinforce his ties to his native continent. He got on the board of the Seattle branch of the United Nations Children’s Fund (UNICEF) and became a trustee of the Africa-America Institute, a New York and Washington-based educational group fostering ties between the U.S. and African nations.
And, most importantly, he has become the American president of the Nelson Mandela Foundation, started by the South African leader to promote education, democracy and health care improvements in Africa.
“As president of the Foundation, I really became exposed to the immense issues and problems of health care in Africa,” says Judja-Sato. “There has been amazing progress, but clearly there are enormous problems still to face.” For instance, he says, 80 percent of African children are not immunized for any diseases. Nearly two million die every year from diseases that could be prevented by simple vaccinations.
“What is amazing is the vaccines are there and people are willing to find them and take them, but when I looked at the problem seriously, I discovered it was a dependable distribution mechanism that was missing,” he says.
VillageReach is Judja-Sato’s solution to the problem. By piggy-backing on existing transportation and communication venues, he hopes to open up Africa to better health care and, he feels, a far better future. For instance, if the Coca-Cola truck can get to a village, there is no reason Coke can’t be induced to have it carry some vaccines as well. Transport companies want roads built for other reasons, so perhaps they will realize that healthy bodies in the jungles will provide good labor for them.
“We want to build strategic alliances, just like in any good business venture,” says Judja-Sato. “We want to show the multiplier effect of good health for economic good. Healthy people and those with healthy families work harder. They are more productive. Women who don’t have to worry about their children become active members of the community. There is less money spent on health care and more on schools and businesses.
“Let me explain my rationale,” says Judja-Sato. “I am an African and fortunate to have a good education and a good job. I have been exposed to wealthy individuals and have access to moral and political leaders like President Mandela. I have to take advantage of these unique circumstances to help solve problems of people in vulnerable and disadvantaged communities.”
Judja-Sato says he has had pledges of funding from the Mandela Foundation, as well as the Bill and Melinda Gates Children’s Vaccine Program and the Craig and Susan McCaw Foundation. VillageReach is still in the nascent stages as Judja-Sato continues to secure funding and build a network of supporters.
“But the important thing is that we have to treat this as a business; otherwise it won’t work. We have to establish sustainable operations that engage local entrepreneurs, support their growth and enable them to create wealth in their communities. We have to make those alliances with governments, international development agencies, transport companies, and entities like World-Vision, Save the Children and CARE. That is what my business expertise offers. I am an entrepreneur. I build alliances,” he says. “I want to be the Fed Ex of remote medical care. If we are successful, it will help Africa to start to get in step with the rest of the world.”
David Brailer: Napster in a Clinical Health Setting
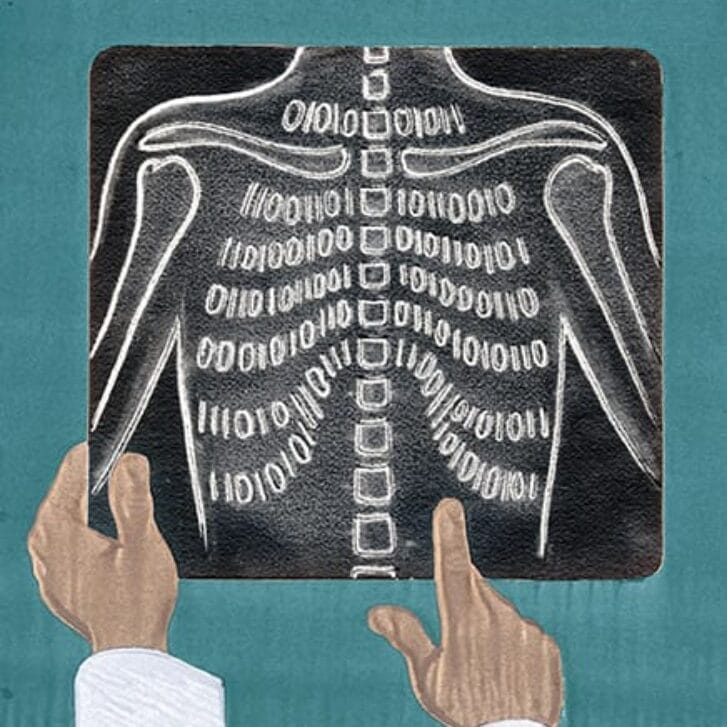
Often statistics are the bane of those who believe that medical care cannot be quantified. But Dr. David Brailer, Gr’92, has a mission to dispel that fear. Brailer is the CEO of CareScience.com, the premiere online medical data sharing service.
“When I was in the doctoral program at Wharton, I spent most of my time in the decision theory group,” says Brailer. “The research projects I was on were all about trying to improve the quality of care and trying to identify problems that patients had, trying to reduce errors.”
The idea was to make health care delivery as efficient as manufacturing had become in the early 1990s. “But we wanted to do this in real settings, not just in laboratories. We needed to have those real settings to know if our ideas on efficiencies could work,” he says.
 To that end, Brailer and his partners set up a non-profit organization to help along those research projects and then spun off a for-profit company, CareScience.com, in 1995 to collect, apply and store all sorts of clinical data for doctors, hospitals and pharmacists.
To that end, Brailer and his partners set up a non-profit organization to help along those research projects and then spun off a for-profit company, CareScience.com, in 1995 to collect, apply and store all sorts of clinical data for doctors, hospitals and pharmacists.
“Basically, we’re Napster in a clinical health setting,” says Brailer, comparing CareScience.com to the Internet music-sharing site. To explain the CareScience.com system, Brailer took a fictional Mrs. Jones. Mrs. Jones has gone to her family doctor for years. He inputs various drugs she has taken for diseases or various procedures for other ills, what has worked and what has not. Her specialists have done the same, and her pharmacy also has input whatever it has given her over the years.
Now, Mrs. Jones is rushed to the emergency room at the University of Pennsylvania health system. Because her doctors are aligned with the system, the hospital has clearance to go in and access her data. Just as they were about to give her a certain medicine, they discover through the data that her doctors have input that Mrs. Jones has had a bad reaction to it in the past. A possibly costly medical error, in both human and financial ramifications, is saved.
Then there is the collective value of the CareScience.com system. “We’re gathering data from a wide population,” says Brailer. “Now you can compare what you might prescribe for a patient to what everyone else has done. Here’s what you may do differently. These things had impacts and these things turned out negatively this or that many times. “Physicians can’t always intuit his or her way to good medical care. The pressures on them to improve care are ones that turn punitive when they can’t figure out what to do. Our data is one good way to help physicians and other health care professionals.”
Brailer says CareScience.com has been used in more than 100 million patient contacts in the last year. It has stored more than 10 terrabytes of information on its servers. “We need pretty powerful computers,” he says, claiming that Care-Science. com is the largest health care warehouse on the world wide web. The company has 140 employees with offices in Philadelphia and San Francisco. Its best customers, according to Brailer, are in areas where the managed care markets are more competitive, like the Pacific Northwest, Minnesota and the San Francisco area; but, of course, the home University of Pennsylvania health system is also a client.
“Our focus is to improve health care for average people,” says Brailer. “Treating errors is more expensive than preventing them. We believe that having this data online will continue to save money and, more importantly, give patients better health care.”
 Elayne Howard: CAM’s Time Has Come
Elayne Howard: CAM’s Time Has Come
Time was when hospitals and other health facilities always toed the straight and narrow. There were certain ways to cure diseases, fix psyches and generally administer patient care. The health care business was among the most stodgy and uptight you could find anywhere.
But Elayne Howard, WG’76, feels there is getting to be room for change, and she hopes she can help those health service providers to move in that direction. As owner of Elayne Howard and Associates, Inc., a suburban Philadelphia health care marketing firm, Howard says she is excited about encouraging health systems to make more use of CAM, the acronym for complementary and alternative medicine.
“It goes by other names, too, like integrative medicine,” she says. “But whatever it is called, it used to be shunned. Yet now, we’re finding that a lot of hospitals feel it is not that foreign an idea.” CAM is just one of a long list of medical ideas Howard has helped health care institutions and pharmaceutical companies market since she got her MBA from Wharton in 1976 in health care management. She first worked at St. Christopher’s Hospital (now a part of Tenet Health Systems) in Philadelphia and then in 1980 went to Shared Medical Systems. In 1988, she decided to start her own company.
“I really had an entrepreneurial itch,” says Howard. “I put together the things I found most stimulating and rewarding – working with clients and doing strategic marketing. To be able to do that in the health care field, where we can help so many people, has been intrinsically rewarding.”
More often than not, Howard says, she does not do public relations, but works with clients to develop strategies to market products or services and to understand what their own clients or patients really need.
“It is a tense and stressful time for the health care industry and that would apply to companies as well as providers,” she says. “There are a lot of pressures on cost. And at the same time, consumers are becoming more sophisticated, because of technology and information, and have higher expectations of services that seem to be the latest and greatest.”
And one of those things patients appear to clamoring for is more access to alternative therapies and health care practices. “Using meditation in support groups, using acupuncture for pain, using alternative therapies for cancer patients – there are tremendous benefits there,” says Howard. Furthermore, health care institutions are finally realizing that not only do these therapies attract patients who want them, they are often cost-effective as well in helping patients be psychologically and physically ready for more traditional care. “It’s an up-and-coming area and something we think providers should be involved in. The only thing is convincing them that an alternative therapy doesn’t mean witch doctors. I’m happy to convince them that it does not, that nutritional therapy and yoga and relaxation methods and massage are all good, even necessary, things for the health care industry today,” she says.