John Smithwick WG01 has been working on his digital health care venture for almost five years—enough time for his company, RoundingWell, to transform into something far more than the patient readmission avoidance tool he originally planned.
Like many in digital health, he has a career that’s bridged two worlds: software and health care. After he finished up at Wharton, he worked at a software firm in Philadelphia and then for four years at Microsoft in Redmond, Washington. He followed that up in Nashville, working for the Tennessee-based disease management provider Healthways. There, in the late 2000s, he found his entrepreneurial opportunity in a study that revealed that $2 out of every $3 spent on hospital patient readmissions could and should have been avoided (in total, hospital readmissions cost $30 billion in the U.S.).
“Across the industry, this study was greeted with universal head nods of agreement,” he says.
This was about the time that health care reform was becoming reality, and health care leaders knew penalties were on the horizon for readmissions courtesy of the Patient Protection and Affordable Care Act of 2010. Yet the health care industry, tied to a fee-for-service business model dependent on patient volume, seemed powerless to do anything about significantly lowering readmission rates, or to avoid the penalties.
Smithwick teamed with his co-founder (now RoundingWell’s chief technology officer) Will Weaver, a product expert and systems architect, and they devised a digital platform that could connect a patient with a hospital team. RoundingWell was originally a patient self-reporting tool that could warn hospital teams if a patient was at risk of readmission. Smithwick and his team recruited hospital systems to test the platform on post-acute and chronic-care populations—people with pulmonary, heart or kidney disease.
“We made some early bets on the Web as a modality to engage patients,” Smithwick says, adding that such an approach ran counter to early industry feedback they received that “my grandma and grandpa would never go online for care.”
How wrong conventional industry wisdom turned out to be.
“We see 60 to 70 percent rates of sustained patient engagement across all demographic categories,” Smithwick reports now, claiming that “no one who tries to engage patients can touch that.”
A needed pivot, however, occurred on the clinician side. At first, RoundingWell’s approach toward medical practitioners was “less is more”—so as to not burden nurses and doctors with yet another complicated technology.
But as Smithwick and his team started testing the platform with larger patient populations, they realized that more functionality was actually a good thing—for case management and care coordination, in particular. They have hospital system customers who actually deprioritize patient engagement and instead focus more on care coordination among a patient’s multitude of caregivers, which is the model toward which U.S. health care is headed overall, Smithwick adds. It’s the “collective delivery of care,” he describes it.
For decades, hospitals lacked an integrated care management platform. So why not transform RoundingWell to become one?
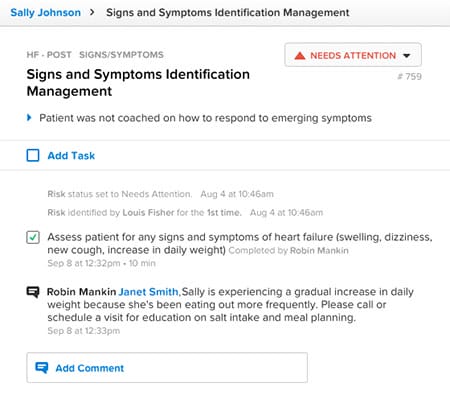
RoundingWell is doing just that. The platform allows hospitals to know what risks are occurring that impact care, as well as how and when they occur.
Smithwick, who married his Wharton sweetheart Josephine WG01, can feel the momentum accelerating as client conversations have changed. Last year, hospitals showed “polite interest.” Now, they are coming to him; hospitals are signing risk-based contracts with insurance companies—collecting fees based on outcomes, not the old fee-for-service deals. To make sure they deliver cost-effective care, the hospitals need care coordination and patient communication platforms. RoundingWell now has a presence in two out of the three largest renal care companies in the country. It’s deployed the platform across some of the nation’s largest hospital systems and is working to partner with several large accountable care organizations. RoundingWell is also taking part in several Medicare demonstration projects, with the hopes of increasing the engagement-based involvement model in renal, cancer and hospice settings.
With thousands of patients on their system and a couple million dollars in funding from private sources (including Wharton grads from a mix of years), Smithwick sees nothing but more opportunity in the current health care environment. Even the company’s physical space—a rehabbed, two-story, redbrick bank building in midtown Nashville where 20 employees currently work—speaks to their market. It’s within walking distance of five current clients.
“We really did underestimate the extent that practitioners would respond to a care coordination platform,” Smithwick says.
That’s a good problem to have. Let’s see where it takes him in the next five years.