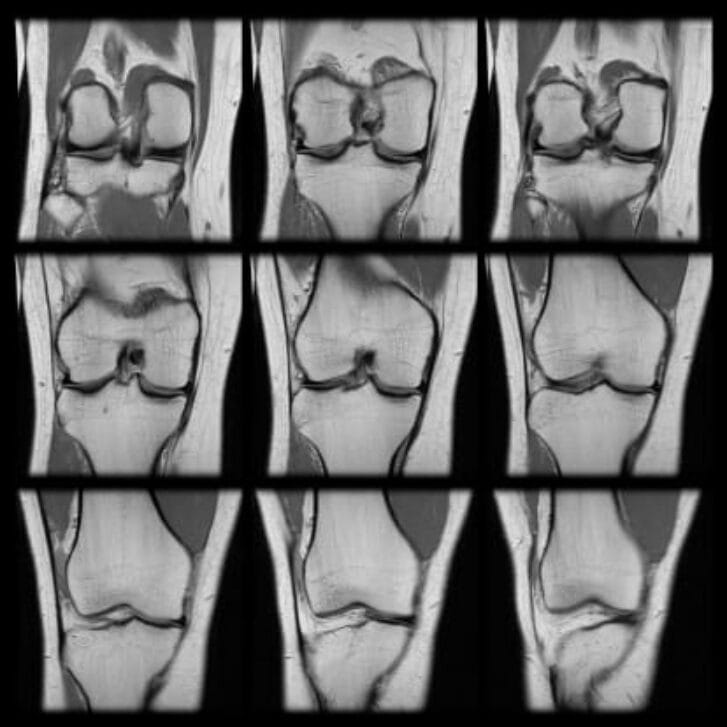
As someone who has worked in the medical device field for over 26 years, I have been amazed at the technologies that have been developed to help improve outcomes in patients. For me, I have witnessed technological innovation in interventional cardiology, orthopedics, cardiac rhythm management, diabetes and various types of diagnostics. While medical device development has slowed considerably over the past several years, their effect on improving outcomes continues. Yet this slowing in innovation concerns me.
What’s stymying development? Recent articles in Health Affairs point to the difficulty in accessing capital and the burden imposed by regulatory and payment processes for these types of technologies. (See a recap in the Health Affairs Blog, “How to Restore the Innovation Ecosystem for Medical Technology.”) Venture capital funding has slowed considerably for medical devices, for instance, in part due to federal government regulatory and payment issues, as well as the flow of funds from venture capital toward other “hot” areas such as health IT. Certainly, there is promise in the use of health IT in improving outcomes. However, I believe this is in the longer term, not in short term.
The question becomes: How patient will venture capital firms be with their typical investment time horizons of five to seven years?
My guess also is that the data breach at Anthem Wellpoint may put a damper on information technology investments. From personal experience and the use of electronic medical records (which are supposed to reduce costs and make care more efficient), I also don’t see electronic health records driving investment happening in the short term. This personal experience includes a recent outpatient procedure at an ambulatory surgery center where I signed over 50 pages of hard copy documents. Nowhere could I find an electronic record.
Health Affairs also reviews how the U.S. lags relative to other developed countries in approving for payment innovative technologies. In the past 15 years, only 19 innovative medical technologies have been approved for additional payment in the hospital inpatient setting. Since the payment amount for these new technologies is less than their cost, hospitals tend not to use them, significantly less than projected by Medicare (CMS). Health Affairs offers recommendations to CMS, such as the use of cost/benefit analysis (where societal benefits exceed the costs) and retrospective adjustments of payments for new technologies, especially where the hospital has lost money.
As someone who is working with a number of medical technologies that provide value to the system but are having difficulty in procuring the capital to grow, I hope misfires in hot investment areas such as health IT will result in venture capital fleeing back to medical devices. Continued coverage in leading health policy journals of these issues, with recommendations on how to fix them, will also help.