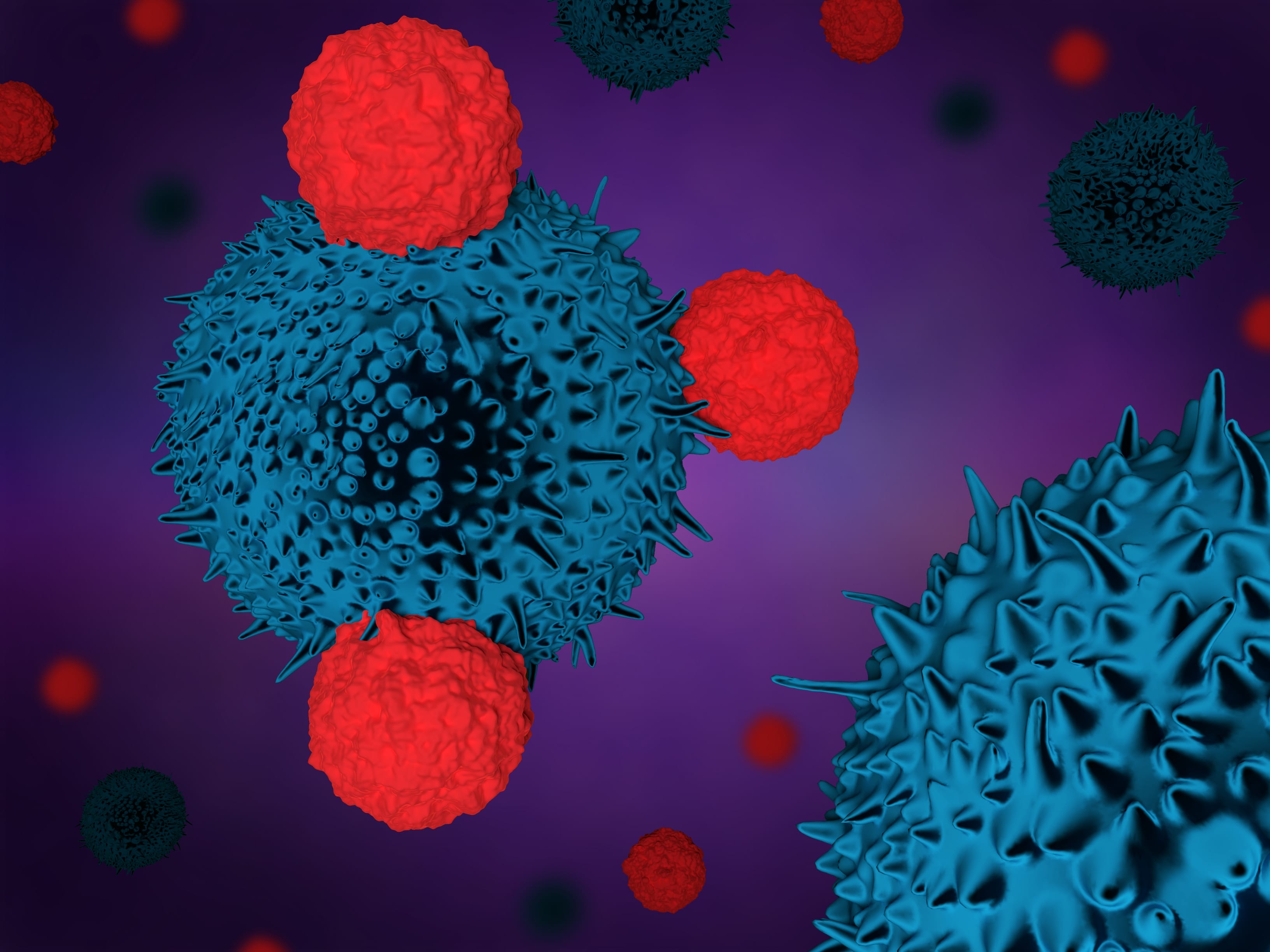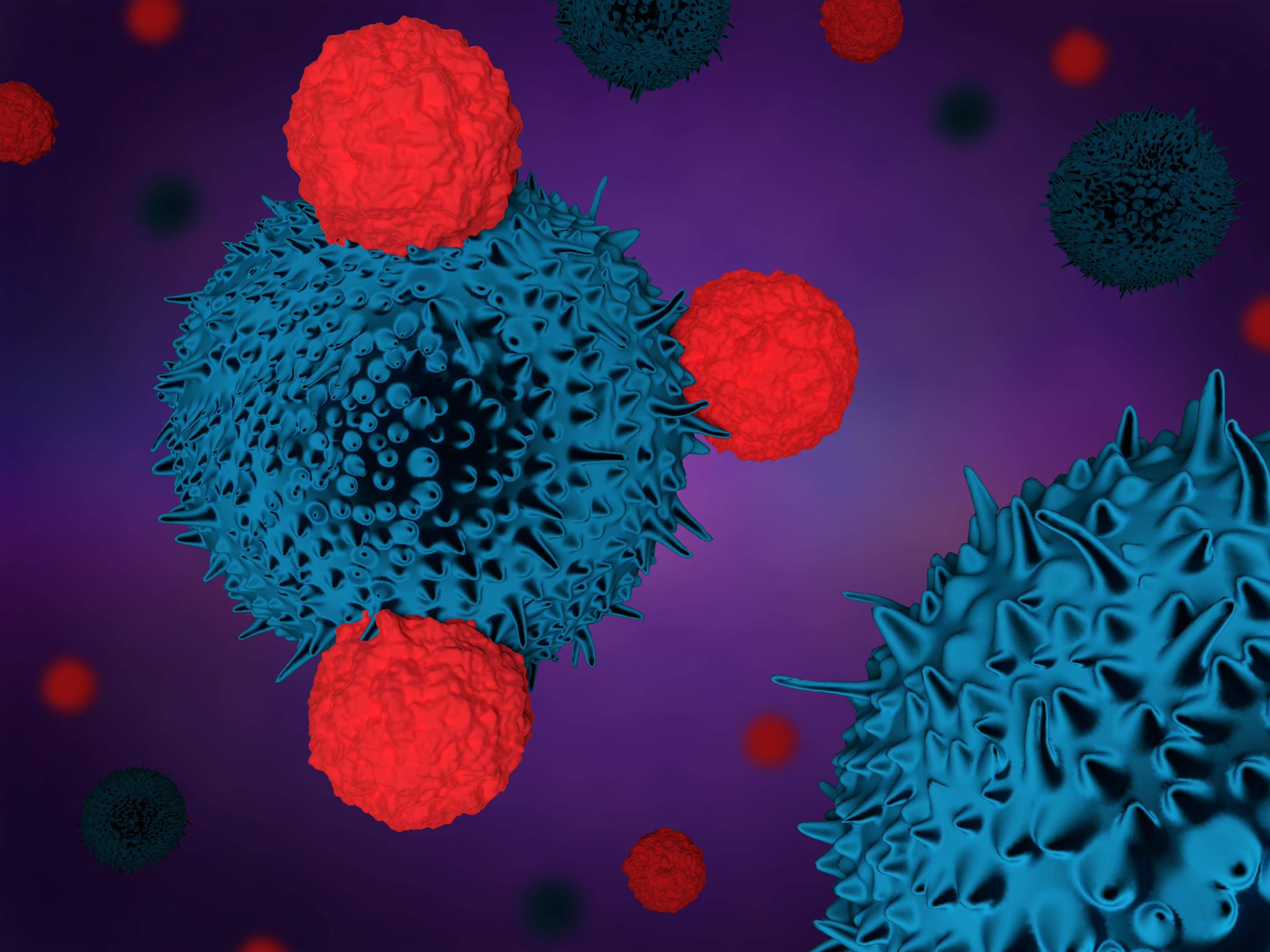
T cells fighting cancer (Getty Images)
On February 13, 2018, I had the opportunity to speak with three of the nations experts on immunotherapy for treating cancer on SiriusXM channel 111’s “The Business of Health Care” radio show. Simply put, immunotherapy supercharges the body’s own immune system to help it fight cancers. Immune cells are extracted from the body, programmed to identify specific cancer receptors, and then injected back into the body to attack hematologic cancers, where they have found the most success. The health care company Novartis has developed this therapy in collaboration with Penn Medicine. The therapy is currently sold in the U.S. and costs about $475,000 per treatment. Novartis has also established outcome based pricing, whereby if the therapy does not work, the patient is not charged. However, it appears to work in 70 percent of patients. Solid tumors are a bit more problematic, however, and this was the focus of our discussion.
Physicians Robert Vonderheide, Gerald Linette, and John Wherry have been working collaboratively to understand how the body’s immune system responds to cancers—especially solid tumors such as non-small-cell lung cancer (NSCLC) and breast cancer. This group’s goal is to not just treat solid tumors but to develop vaccines that can prevent cancers from occurring in the first place. Solid tumors have been difficult for the body’s immune system to fight for several reasons. The tumor’s micro-environment inhibits and suppresses the body’s immune response using a protein called programmed death (PD-1). PD-1 is problematic in this case because it blocks the T cells from getting to the tumor. These clinicians, in addition to developing T cell therapies, have also been identifying and developing therapies to block inhibitors such as PD-1, which would allow the T cells to attack the solid tumor.
The tools immuno-oncologists such as Dr. Linette and Dr. Vonderheide have at their disposal now include traditional cancer drugs, radiation, check point inhibitors, and T cell therapy. These methods of treatment provide very powerful therapies to eradicate a tumor or keep it in check. An integral part of the process is supercomputing, used to identify the cancer mutations in a patient. While this identification is key to immunotherapy, it can cost hundreds of thousands of dollars, making it inaccessible to many.
The holy grail for immunotherapy is preventative cancer vaccines, which will likely cost significantly less than current therapies. These vaccines would train the immune system to identify mutations as the cancer begins to develop, and kill them. There are several clinical trials underway at Penn Medicine for patients with breast or melanoma cancers. Imagine that a female patient is diagnosed with the BRAC1 and BRAC2 gene mutations—meaning she is at high risk for breast cancer—in her twenties. She has children and in her late thirties is injected with a cancer vaccine which identifies this mutation when it begins to express itself in breast cancer and kills the mutation. Thus the patient is immune to this type of breast cancer.
T cell therapies and vaccines are in their infancy. The cost to manufacture these types of patient specific therapies are significant. However, a nascent industry is developing around the manufacture of these therapies which will evolve over time and likely bring down the costs, making it more affordable for the health system. This is an exciting time in cancer therapy and clinicians like Vonderheide, Linette, and Wherry are leading the way towards durable cures for these types of cancer.
[Editor’s note: This post has been updated to include audio of this “Business of Health Care” episode, which you can listen to with the link below.]