There’s no doubt that aspects of the United States’ health care system are ailing. Millions of working people are uninsured, access to services varies widely, and Medicare is predicted to reach a crisis in coming years.
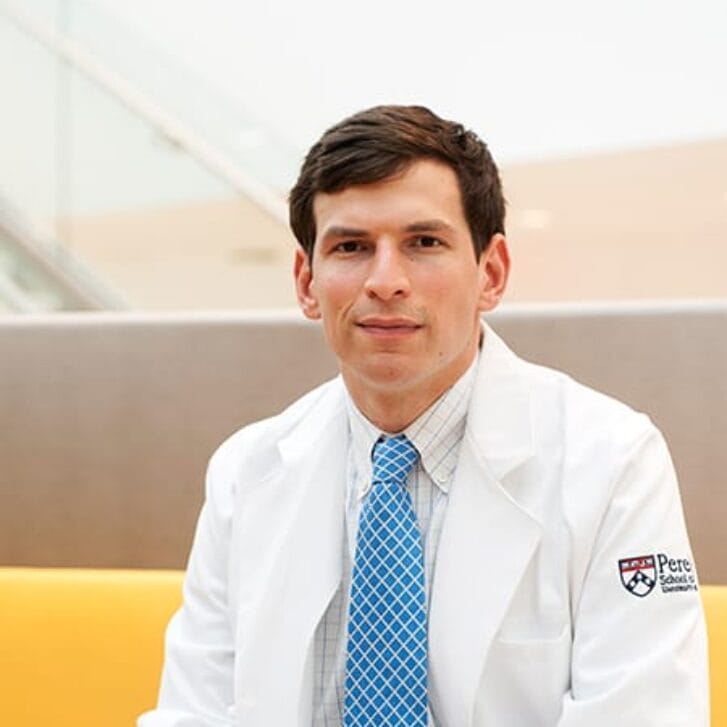
No one is better suited to help heal the system than Risa Lavizzo-Mourey, MD, WG’86. As the president and CEO of the Robert Wood Johnson Foundation (RWJF) since 2003, Lavizzo-Mourey applies principles she has learned from her training in business, medicine, and public policy to guide strategic investments that redesign systems and improve the health and health care of all Americans.
From a career as a practicing physician and work in academic medicine, she moved into the public sphere as an expert in health care policy, held positions in government, and played a key role in philanthropy. After earning her medical degree from Harvard, Lavizzo-Mourey went on to earn her MBA at Wharton. At the Medical School of the University of Pennsylvania, she served as a Robert Wood Clinical Scholar, where she specialized in geriatric medicine. While at Penn she became the Director of the Institute of Aging and the Sylvan Eisman Professor of Medicine and Health Care Systems.
While the Foundation’s $9 billion in assets makes it the nation’s largest philanthropy dedicated exclusively to health and health care, its resources are dwarfed by the scope of the need. Under Lavizzo-Mourey’s leadership, the Foundation refocused its priorities and restructured its grant-making activities into an “impact framework.” This framework brings more integrated strategies to a highly targeted set of program priorities.
The framework clusters the majority of the Foundation’s grantmaking into four strategic portfolios: Human Capital, Vulnerable Populations, Pioneer, and Targeted. Like an investment fund, each portfolio targets specific high-impact goals, seeks results across different time frames, and assumes varying levels of risk. Human Capital aims to develop a diverse workforce of health care leaders and practitioners; Vulnerable Populations addresses health and health care problems that intersect with social factors like poverty, race, education and housing; Pioneer invests in innovative and cutting-edge programs that often involve high-risk; and the largest of the four, Targeted, addresses the urgent need for short-term action with long-term impact in eight areas — health care coverage, nursing, childhood obesity, health care quality, disparities in health care, public health, tobacco, and addiction prevention and treatment.
The problems Lavizzo-Mourey aims to solve are indeed big — bigger than any single leader or even any private foundation — but she is able to recognize issues on a system level, understand the individuals affected, and bring together the people and organizations needed to make a difference. As committed to healing individuals as well as society, she still treats patients at a community health clinic in New Brunswick, NJ.
Lavizzo-Mourey says of herself: “What continues to energize me is the opportunity to address big problems in the area of health and health care, to make a difference on a large scale, and to touch people directly and change their lives.”
Why did you change your path to philanthropy?
I grew up as the daughter of two physicians and intended to have a career as a practicing physician focused on individual patients and their health care. While I never envisioned a career in philanthropy, in hindsight it was a natural progression.
My personal connection with philanthropy began as a Robert Wood Johnson Clinical Scholar at Penn. Certainly, that initial connection with philanthropy, with the Foundation I am now privileged to lead, has taken me down paths I could not have imagined when I arrived in Philadelphia in 1982.
Philanthropy at its best can be transformative — changing the lives of its beneficiaries as well as changing the trajectory of entire neighborhoods and communities, changing entire systems, changing public policy and private action. My background and experience in various aspects of medicine, business, academia, and government, give me a unique perspective and understanding of these different fields. For example, the lessons I learned at Wharton help me apply concepts from business into health care. I can also help the Foundation serve as both a convener and bridge between the different fields and areas we are working.
It takes a multidisciplinary approach to attack root causes head-on and transform the health care system and with it, society as a whole.
Given the unequal access and inferior health care of racial and ethnic minorities, what steps can be taken to reduce these disparities?
It’s important to recognize that a lot of people don’t appreciate that Americans from different racial and ethnic backgrounds are not getting the quality of care that they should. I have been thinking about and writing about this area for a couple of decades now. In fact, a few years ago I had the opportunity to co-chair The Institute of Medicine’s Committee on Racial Disparities in Health Care.
The Foundation’s strategy is focused on finding and implementing practical, evidence-based solutions that target diseases where both the evidence of racial and ethnic gaps and the recommended standard of care are clear. What we are realizing is that when you bring those two characteristics together, you begin to see not only changes in attitude but also real gains. These gains are not just in reducing disparities, but in improving the overall quality of care as well.
And that really is the kind of work the Foundation is doing, working on testable ways of solving the problem. I am heartened by the fact that there are signs that we are improving the quality of care and narrowing the disparities gap in some areas.
Many children in our country are significantly overweight. What strategies might be effective in dealing with this epidemic of childhood obesity?
If the trend in childhood obesity continues, we are in danger of raising the first generation of children who will live sicker and die younger that their parents. Fortunately, there are a lot of strategies, and a handful of approaches that I am confident will help halt the rise in childhood obesity.
Children have to learn healthy lifestyles in their current environment. Average American lifestyles have become incredibly sedentary. It is hard for many people to make the healthy choices that they want to make. It is hard for them to find healthy foods and to integrate physical activity into their lives so that it is not an extra activity but just something that is done every day. So what we are trying to do through a coordinated effort is to improve the environments for kids so that they think of healthy choices as normal choices, as the right choices.
RWJF has a four-pronged approach to halting the increase in childhood obesity. We are building the evidence regarding what works to promote healthy eating and physical activity among kids; testing innovative approaches so we can spread promising models; educating leaders and investing in advocacy strategies; and working on ways to help health care providers screen and counsel to prevent and manage childhood obesity.
We are very much committed to building evidence and testing innovation. For example, RWJF has provided grant support to the Food Trust of Philadelphia, which operates a network of community-based farmers’ markets, school markets and nutrition education programs to address diet-related health problems in America’s lower-income communities. Its Corner Store Campaign is teaching children to make healthy choices at corner stores that are close to schools, and offers an incentive system to encourage them to buy healthy snacks as opposed to non-healthy snacks. And that innovation has been shown to work over the long term.
You have urged doctors to resume the old practice of making house calls in order to see how patients live and to cut back on emergency room visits. Are there other new “old” ideas that you would recommend?
Benjamin Franklin had it right, “An ounce of prevention is worth a pound of cure.” We could bring down health care costs dramatically and improve the length and quality of life by having a society that is more healthy and committed because it is fit.
Another “old idea” that dates back to Franklin and beyond is having a health care provider who is part of the network and social fabric of a community. At the Foundation, we refer to them as the front-line workforce, the people who are actually doing the hardest job — the most direct care with the patients. They are members of the community who help break down the barriers that often prevent people from feeling like that they are getting care appropriate for their culture, that is meaningful to them, and has the continuity they want and need. Connecting health care providers to the communities they serve bears revival.
A very old concept that is particularly relevant for our work with childhood obesity, is creating a healthy environment for people to get back in touch with the equations about how the energy we put in has to be matched with the energy we burn. The proportions are now one and a half times what they should be, and the amount of energy that we are able to burn just doing our regular day-to-day activity has diminished to basal levels.
What advantages do you see in examining patient populations rather than individual patients?
While there is nothing like connecting with a patient one-on-one and doing everything within your power to help that person, there is only so much you can do in that one visit or through the doctor-patient relationship.
For example, think about some of the work that has been done to reduce the prevalence of tobacco use. As a geriatrician, I frequently treated patients with health problems that resulted from a lifetime of tobacco use and exposure. As a physician there was little I could do. However, at the Foundation, we have an opportunity to think about making root changes: having smoke-free work environments, taxing cigarettes, or setting the price of tobacco so that it is a deterrent to smoking. By combining all those things, we can help millions of people lead longer and healthier lives. For me, it’s like going from singular to plural.
When we take all of those societal or system-wide opportunities for changing the population’s health and combine them with what individuals can do with one single patient, we really have the opportunity to transform society in major ways.